Sedating Babies With Food
Words like unethical, harmful, and concerning come to mind when considering the idea of parents dosing infants with sedatives to prolong sleep for their own benefit. Such actions prioritize adult convenience over the well-being of the child, raising serious moral and health concerns. As a parent, being advised by trusted individuals to use drugs on a baby for better sleep would invoke feelings of anger, fear, and confusion. The health and safety of my child is paramount, and the thought of compromising that for my own rest is deeply troubling.
Reflecting on past practices, such as introducing solids too early or adding ingredients to formula designed to override natural appetite cues, also raises significant alarm. These actions could be viewed as neglecting a baby’s developmental needs in favor of misguided attempts at convenience. If I were to receive such advice from someone I trusted, my response would be one of skepticism and concern. I would seek to understand the reasoning behind the advice, educate myself on best practices for infant nutrition and sleep, and ultimately prioritize what is healthiest for my child, even if it means standing firm against popular or outdated recommendations.
Some parents still hear that they can make their baby sleep better by giving them extra calories or using sleep-inducing substances. Some infant formula companies even promote "special" products claiming to help babies sleep.
Anything given to babies beyond breastmilk or formula in the first six months should only be done with medical advice. This advice must be well-informed. Health professionals follow guidelines for infant feeding and for medications, whether prescription or over-the-counter.
Premature Solids
Starting solids too early (before six months) is often recommended to help with frequent night waking, which commonly occurs between 3-6 months. Some people believe that small servings of rice cereal or pureed fruits and vegetables have more calories than breastmilk, but this is misleading. Just a teaspoon or two of these foods provides much less energy than breastmilk or formula.
A common solution is to give the baby formula at bedtime, either along with or instead of breastmilk, to help reduce nighttime wake-ups. "Dream feeds" let you feed the baby without waking them, similar to refueling a car while it's still moving.
So what is the evidence supporting these techniques? Do they make a difference and what risks are associated with their use?
A study published in 2021, Type of Milk Feeding and Introduction to Complementary Foods in Relation to Infant Sleep: A Systematic Review looked at the issue:
“This review compares how different types of milk feeding affect sleep in infants under 12 months. Exclusively breastfed infants (under 6 months) tend to wake more at night than formula-fed infants, but this pattern doesn't apply to those who are partially or mainly breastfed. Most studies showed no significant difference in night-time sleep or total sleep over 24 hours between exclusively breastfed and formula-fed infants under 6 months. However, after 6 months, many studies indicated that breastfed infants sleep less than formula-fed ones. Limited studies did not find a link between when complementary foods are introduced and total sleep duration, even comparing those introduced before and after 6 months as per WHO guidelines.”
”More studies should look into sleep factors like the longest sleep duration and how long it takes to fall asleep, particularly how the timing of introducing solid foods affects sleep. There is a need for consistent and better-quality sleep studies in this age group to improve the way sleep is measured, clarify definitions of milk feeding and nighttime, and use more reliable methods for assessing sleep. This will help clarify how infant feeding impacts sleep. Also, to fully understand how different feeding methods and the introduction of solid foods affect infant sleep, future studies should track sleep over time, especially during changes in feeding practices.”
Studies indicate that formula-fed babies often sleep longer than breastfed babies. However, breastfeeding mothers usually sleep longer and find it easier to go back to sleep than bottle-feeding mothers. While bottle-fed babies may wait longer between feedings, preparing a bottle can disrupt sleep more than breastfeeding, making it tougher to return to sleep.
The behavior of formula-fed babies is often seen as "normal," leading to comparisons with breastfed babies. It's important to remember that, like all mammals, humans produce the right milk for their young. Human babies require lighter sleep and regular feeding. This is different from cows and other herd animals, whose babies need to grow strong quickly to stand and walk soon after birth. Their milk helps with rapid development and promotes deep sleep, allowing the mother to graze while the baby rests in tall grass.
Human babies don't walk for about a year after birth, so building bones and muscles isn't a main focus. However, the brain grows quickly and requires frequent breast milk for nourishment. Infants also tend to stay in a lighter sleep because they need to hold on to their mother as she moves. While human milk can calm babies, it doesn’t sedate them as much as the milk of ground-living mammals. Human milk supports human needs; cow milk supports cow needs. Although we can adjust cow and animal milks to be easier for humans to digest and add vitamins, we can't remove the stronger proteins and sedative effects. More isn't always better; babies not breastfed face a higher risk of Sudden Infant Death Syndrome, possibly because they sleep too deeply and lack maternal contact to encourage regular breathing.
"In fact what constitutes normal and healthy infant sleep cannot be understood independent of nighttime breastfeeding as the two co-evolved and was designed by natural selection to maximize infant health and well-being."
Dr James McKenna
“Encouraging a baby to sleep too deeply, too soon, may not be in the best survival or developmental interest of the baby. This is why new parents, vulnerable to sleep trainers' claims of getting their baby to sleep through the night, should not feel pressured to get their baby to sleep too long, too deeply, too soon.”
Dr William Sears
Many believe that fathers will share feeding equally, but they usually only give one bottle a day, often not at night. If you think bottle feeding will help you sleep more, that's unlikely. When a breastfeeding mother says she's tired from a restless baby, she often gets sympathy and suggestions to switch to formula. However, when a formula-feeding mother shares the same issue, responses are usually indifferent.
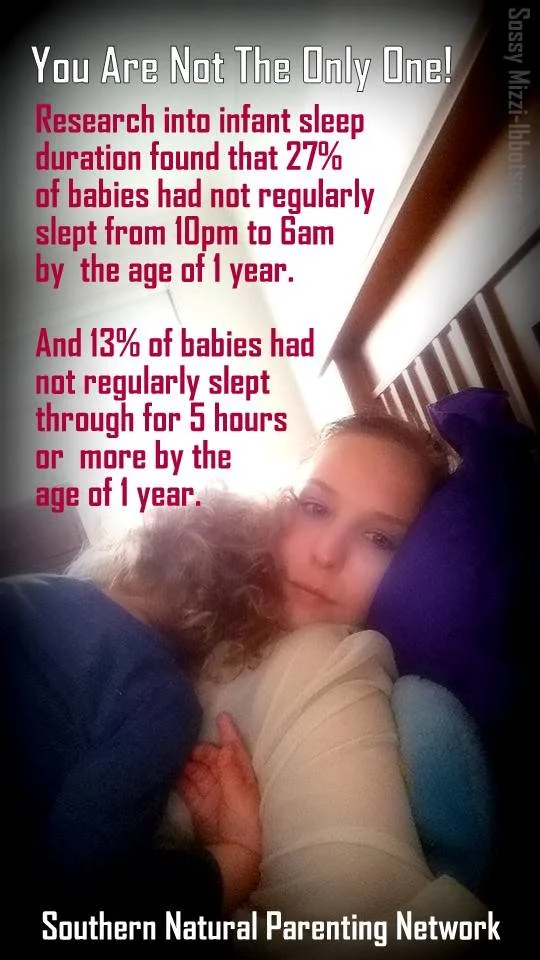
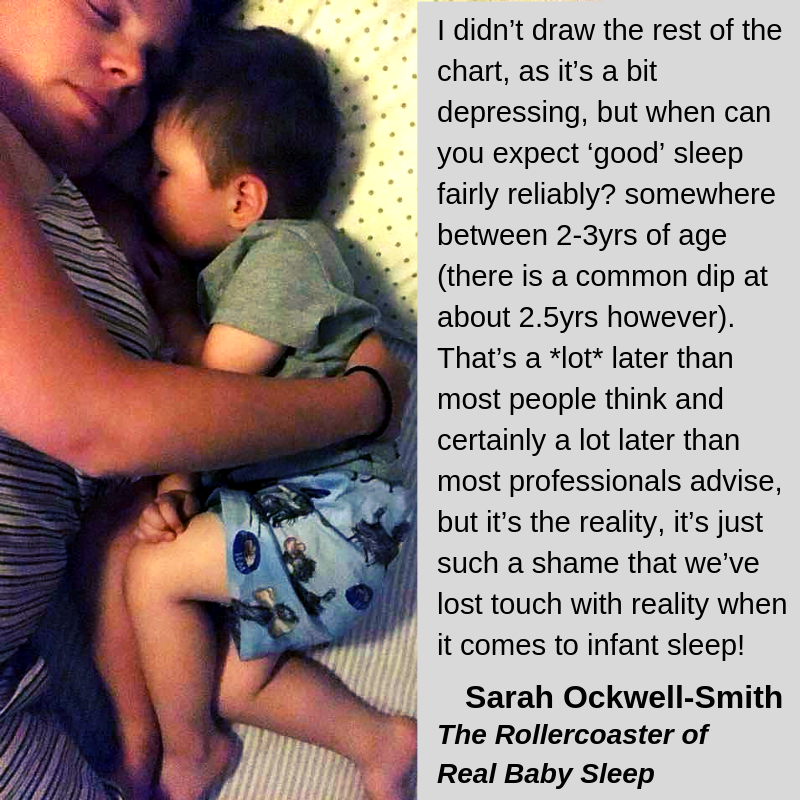
Sarah Ockwell-Smith, author of best-selling books including The Gentle Sleep Book addresses the normal progression of infant sleep in her article The Rollercoaster Of Real Baby Sleep. The data is a reality check for parents:
As it happens, 3 months is the peak of sleep in the first year, that means it’s as good as it gets. There is a very, very high likelihood that your baby will sleep the best they are going to sleep until their first birthday (and later) around the age of about 3 months. It’s really not uncommon for 3 months to be happy to be put down, to only wake once or twice in the night and to go to sleep easily after a quick feed/cuddle.
Then 4 and 5mths happen, they’re not fun months. You get lulled into a false sense of security at 3mths, then suddenly your baby is waking every hour, won’t be put down and is awake for an hour or more refusing to go back to sleep. This is normal development, it is temporary and you didn’t do anything wrong! You also don’t need to do anything to change it, keep doing what you’re doing. Don’t be scared of bad habits and especially don’t consider sleep training. It’s temporary!
You often get a blissful little blip of better sleep around 5-6mths, then just when you think “finally, it’s getting a bit better”, bam, thinks get worse again, usually not as bad as they were at 4mths, but still far worse than you’d hope.
Thankfully from around 11mths things start to improve again, fairly steadily for the next 6mths or so (although not the golden heyday of 3mths!). You can still expect nightwaking and night feeds at this age though.
Professor James J. McKenna’s research highlights the complex dynamics of mother-infant cosleeping, particularly with regard to breastfeeding and the risk of Sudden Infant Death Syndrome (SIDS). His findings indicate that when adults and infants share a sleep space, both parties tend to enter lighter stages of sleep and wake more frequently. While this lighter sleep might initially seem unfavorable, it allows for increased opportunities for caregivers to monitor their infants and ensures that babies can adjust their breathing in sync with an adult’s breathing patterns.
Additionally, McKenna points out that this arrangement can lead to longer overall sleep duration for both adults and babies. This is largely because caregivers do not have to fully get out of bed for nighttime feedings, and babies experience less disruption when they are fed promptly. Enhanced sleep quality and quantity can have significant benefits for daytime parent-child interactions. Well-rested parents are often better decision-makers and exhibit improved emotional regulation, which is crucial as sleep deprivation has been linked to an increased risk of postpartum depression.
McKenna’s work further elaborates on the biological interactions during shared sleep. The physiological signals—such as heart rates, brain waves, oxygen levels, and breathing patterns—are shared and mutually influence one another, acting as a regulatory system for the infant who is still adapting to life outside the womb.
Moreover, McKenna's research supports the assertion that room-sharing presents a lower risk of SIDS compared to infants sleeping in separate rooms. However, sharing a room with other children does not have the same protective effect. Overall, these insights underscore the significance of mindful sleeping arrangements for enhancing both infant safety and parental well-being.